Michigan mom sues for disability in latest U.S. legal battle over long COVID

- Michigan woman was a runner, health care manager, and active mom before she contracted COVID-19 in 2020
- After her infection, she said she began having seizures, near-daily pain, debilitating fatigue and a mini stroke
- She’s suing for long-term disability — one in a growing number of cases against insurers that denied disability claims
KIMBALL—In this tidy home where family photos hang on the wall and heart-decorated dish towels hint to the upcoming Valentine’s Day, Kelsey Warshefski appears for a moment like any mom who might be relaxing with her 7-year-old son on a recent snow day.
But Warshefski, who just four years ago was an active mother, busy manager and frequent runner who lifted weights, said she now struggles to get out of bed each morning because of long COVID, according to a federal lawsuit seeking long-term disability benefits.
She said her fingers tremble. Her toes frequently turn purple. Mid-day fatigue forces her back into bed most afternoons at her home near Port Huron. Words — even familiar ones — can seem just out of reach. At 41, she has seizures and mini-strokes. And her once-muscular frame has lost 45 pounds.
Warshefski is among a growing number of people suing over disability denials as health systems, employers and insurers grapple with how to precisely define long COVID, and whether individual cases amount to long-term disability.

The markers vary from person to person and can flicker on and off. And while some of COVID’s lingering problems — blood clots, kidney failure, respiratory issues, rashes and hair loss — are measurable, other symptoms aren’t as objectively provable — brain fog, memory loss and other cognitive impairments, fatigue, anxiety and pain. Some patients, including those in health care professions, say doctors are sometimes skeptical when they describe their symptoms.
Related:
- Long COVID patients, dismissed by doctors, turn to art to show their pain
- Long COVID remains a debilitating medical mystery for Michigan sufferers
Estimates vary on the number of people who suffer from long COVID, in part, because they’ve looked at different populations. One study put the number as high as 65 million people globally. In a U.S. survey, 1-in-5 adults who had COVID said they suffered from long COVID symptoms three or more months past initial infection.
Warshefski’s suit relies on numbers from the U.S. Department of Health and Human Services, which estimates between 7.7 and 23 million Americans suffer from complications after a COVID infection.
The federal government recognizes the condition as a disability under the Americans with Disabilities Act, with about 56,000 disability claims linked to COVID-19 by U.S. Social Security. And the U.S. Department of Labor requires employers to reasonably accommodate employees with long COVID, such as providing flexible scheduling or remote working.
Even so, proving long-term disability through Social Security or an insurance contract can be tricky, said Andrew Wylam, president and co-founder of South Carolina-based Pandemic Patients, a nonprofit that advocates for people with long COVID.
Research is new because the virus and its aftereffects remain fairly new. While a blood test can reveal high cholesterol, for instance, or biomarkers for cancer, “with long COVID, we just don't have that tool yet to say ‘This is how you are impaired,” Wylam said.
“This isn't a broken bone,” he added. “This is maybe a broken immune system.”
And many of long COVID’s symptoms are associated with other diseases.
Even with a diagnosis, it’s another thing altogether to prove that related brain fog or exhaustion, for example, limit a person’s ability to work. The result, Wylam said, is that “insurers are benefitting from that ambiguity.”
‘The fatigue is tortuous.’
Warshefski’s federal suit, assigned to Eastern Michigan District Court Judge Linda V. Parker, accuses Connecticut-based Hartford Life and Accident Insurance Company of breach of contract for refusing Warshefski’s claim for long-term disability.
Some mornings, she said, she cannot get out of bed at all, let alone returning to her responsibility of managing a 100-plus-bed long-term care Trinity Health System facility where she once worked.
The constellation of symptoms “waxes and wanes,” she said, but “the fatigue is torturous.”
Hartford did not return several messages seeking comment. An attorney for Hartford was not immediately available, and the company has not yet responded to the allegations in court. Trinity, which is not named as a defendant, would only confirm Warshefski’s employment.
Warshefski said the fact she was ill — and debilitatingly so — was never in question after she was infected with COVID late in 2020. After working long hours at the height of COVID, facing confused, elderly residents and angry family members who could not see them because of pandemic protocols, she first developed a tickle in her throat.
She pulled into the parking lot of the Sanctuary of Mercy Village, part of Trinity Health, in Fort Gratiot Township one morning. She asked for a test and it was unsurprisingly positive. Staff had already been sick; residents, too.
Warshefski returned home, where she said she slid further into an illness that worsened with each passing day, week and month. Ford, her then-4-year-old son, got sick; her husband, Jason, developed mild symptoms.
But as her family began to get better, Kelsey said she grew worse. Her hands and feet would go numb. Tremors started. Her taste and smell was wrecked. Abdominal pain. Confusion.
Warshefski, the suit claims, is “among a rare category of infected persons who possessed an unusually susceptible immune system and for whom the viral infection wreaked real havoc on her overall health, physically, mentally and cognitively.”
Initially, Trinity granted her medical leave and approved short-term benefits, according to the suit.
But as time wore on and Warshefski’s symptoms worsened, Hartford denied her long-term disability, said J.J. Conway, an employment law attorney from Royal Oak who is representing her.
Warshefski was sitting in the kitchen recently, wearing bright purple Brooks running shoes. She can no longer run, she said, but the shoes offer stability since her now-shaky balance sometimes sends her to the floor.
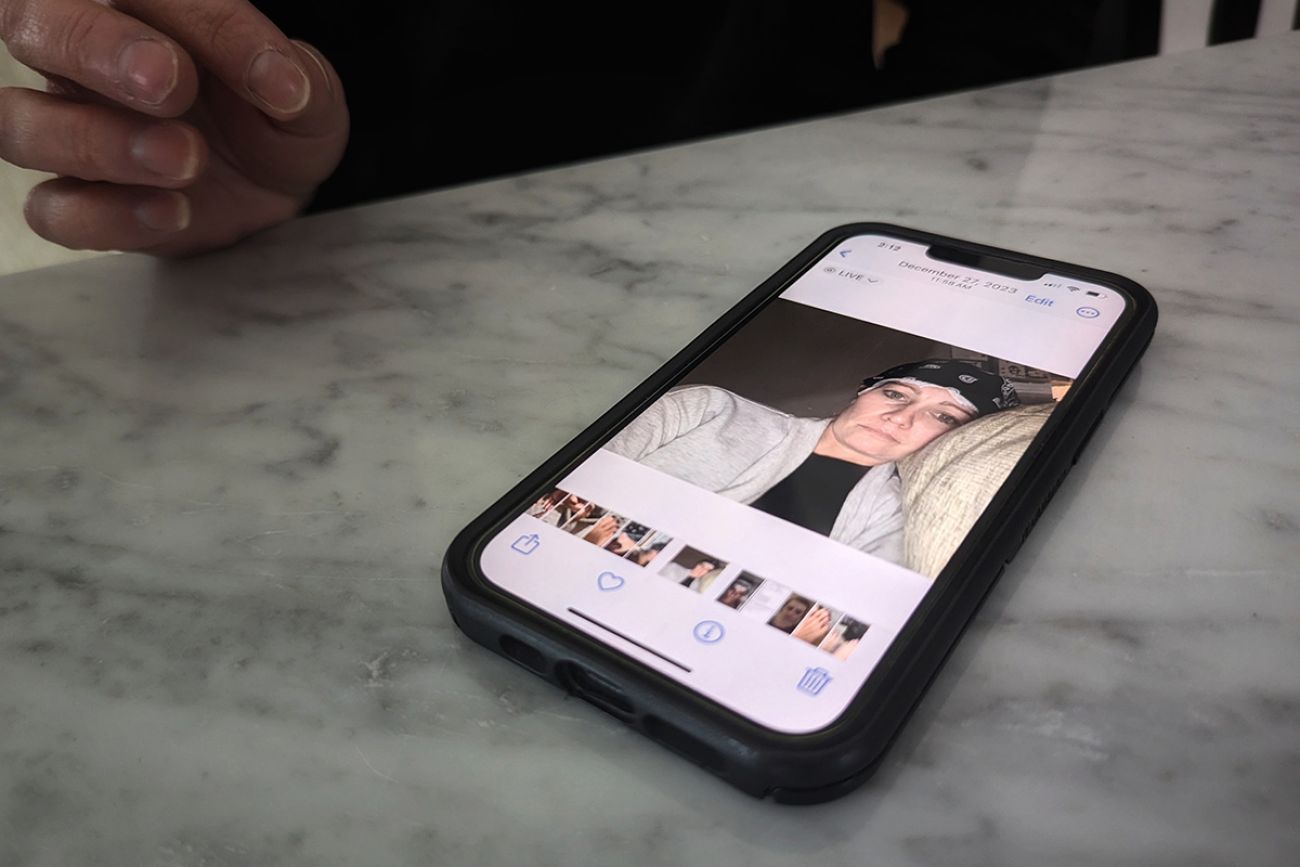
As Ford happily jumps from one chair rest to another, she flips through pictures on her phone — photos of purple toes and selfies in bed or of her in hospitals after a series of seizures.
Warfsheski said she misses work.
She misses the lung-filling air of a good run or a trip to get groceries without fatigue. The ability to jump and romp with Ford. To go to a doctor’s appointment without her mother, a frequent companion these days.
Perhaps most frustrating, she said, is not knowing whether this will end, Warshefski said: “I just want my freedom back.”
Whether her suit will succeed is unclear. Many of the federal suits over long COVID disability claims have been privately settled, making it more difficult to measure their impact. And claimants often have to go through a grueling claims battle with their insurer before taking their cases to court, adding to the burden.
Disabilities rights attorneys say a patient’s odds of success improve when they thoroughly document their health journeys, including daily journals or even videos of their symptoms, such as fatigue, shortness of breath, skin conditions or cognitive difficulties, along with testimonials from colleagues or friends. Other medical experts can be consulted, such as pulmonologists to confirm lung ailments.
Pandemic Patients is one of several organizations that offer advice on how to document long COVID.
See what new members are saying about why they donated to Bridge Michigan:
- “In order for this information to be accurate and unbiased it must be underwritten by its readers, not by special interests.” - Larry S.
- “Not many other media sources report on the topics Bridge does.” - Susan B.
- “Your journalism is outstanding and rare these days.” - Mark S.
If you want to ensure the future of nonpartisan, nonprofit Michigan journalism, please become a member today. You, too, will be asked why you donated and maybe we'll feature your quote next time!





